The panel discussion was chaired by Mr. Javed Jabbar, Former Minister for Information while Ms. Shahida Azfar Chief of Party FALAH Project, Population Council moderated it. Dr. Zeba Sathar Country Director Pakistan Population Council, Dr. Ghazala Mahmud Head of Department MCHC-PIMS, Ms. Katie McDonald Associate Mission Director Democracy & Health USAID and Ms. Khawar Mumtaz Advisor Shirkat Gah were the participants.
Dr. Zeba Sathar gave the initial presentation. She argued that Family Planning (FP) has been wrongly positioned as a stand alone effort and wrongly understood as a means for controlling numbers. Rather it is the cheapest and the most effective intervention for achieving Millennium Development Goals (MDG) 4 to reduce Under-five Mortality Rate (UMR) by 2/3 (between 1990 and 2015), a target figure of 40 per 1000 live births and also MDG 5 to reduce Maternal Mortality Rate (MMR) by 3∕5 (between 1990 and 2015), a target of 140 per 100,000 live births in addition to achieving universal access to reproductive health. She further argued that FP would also help in achieving MDG 1: eradicating extreme poverty and hunger and MDG 2: achieving universal primary education.
Her focus was to convince the audience of the dire need to mainstream FP as a health and development intervention. She first detailed the current reality based on the data from Pakistan Demographic Health Survey (PDHS) 2006-07. The present rate of MMR is 278 which given the current pace will decrease to 220 by 2015, eighty above the MDG 5 target of 140. Similarly the current Infant Mortality Rate (IMR) stands at 78 decreasing to 61 at current pace against the MDG 4 target of 40. Sather’s proposed thesis was that high fertility was the biggest hurdle in achieving MDG 4 & 5 and FP was most effective in reducing unwanted fertility. Thus FP was the most needed health intervention in the country, but current FP programs concentrated too much on controlling numbers rather than on pregnancy spacing and healthy maternal and fetal outcomes.
Wanted Fertility has drastically decreased while Unwanted Fertility has increased over time creating a huge potential for decreasing fertility.
Arguing the first part of her thesis, Sathar presented data showing that Wanted Fertility had drastically decreased while Unwanted Fertility had increased over time creating a huge potential for decreasing fertility. In contrast to 1991 when Wanted & Unwanted Total Fertility Rates (TFR) were 4.7 and 0.7 respectively, in 2007 corresponding TFRs stood at 3.1 and 1.0. Further elaborating, she presented data showing how there was more demand for birth spacing at earlier births while mothers did not likely want more children at later births. After the first birth, 49.9% of women ‘want more children later’ and only 4.1% ‘want no more children’. But after three births the numbers flip with 48.2% women wanting no more births while only 22.8% wanting more children later.
To further hit her point home about mothers not wanting more children, Sathar presented statistics on Unsafe Abortions and their consequences. Out of the total 5 million annual pregnancies in Pakistan, about 1 million (20%) are terminated through induced abortions usually taking place under unsafe conditions as abortion is illegal in the country. These abortions result in 250,000 complications, further leading to 1,500 deaths in addition to the known 11,000 maternal deaths from 4 million births. This provides enough evidence to suggest that there is a need among women to limit their fertility. Thus the question: Is this need being fulfilled and how can it be best met? With only 30% of parents using contraceptives and a Contraceptive Prevalence Rate (CPR) of 36, it can be convincingly stated that the need is not being met.
Specifically regarding mother’s health, Sathar presented strong evidence that lowering fertility is the best means to reduce MMR. Basing scenarios on the current MMR of 276 with General Fertility Rate (GFR) at 135 and Skilled Birth Attendance (SBA) at 39%, she showed that by increasing SBA to 50% while keeping GFR constant, MMR would decrease to 237; by decreasing GFR to 100 while keeping SBA constant, MMR would decrease to 182; but with GFR at 100 and SBA at 50%, MMR would decrease to 156, slightly above the 140 MDG 5 target.
Sathar then shifted focus to IMR arguing that although IMR had decreased quite a bit from 1991 to 2007, IMR had not come down proportionally primarily because of a slight increase in Neonatal Mortality Rate (NMR) during the same time period. Thus stressing the need to concentrate on mother’s health as neonatal mortality was directly linked to MMR. To substantiate her argument, she explained the statistics for NMR and Post-neonatal Mortality Rate based on Birth to Conception Interval (BCI). For BCI of less than 6 month, the rates were103 and 44 respectively, decreasing to 26 and 22 as BCI increased to a 24-29 month period. Thus about 96,600 infant deaths could be limited if the minimum interval was greater than 24 months.
Further, research also indicated the affect of increased fertility on mother and child welfare as demonstrated by the following table.
: Maternal Health Outcomes
| <=3 Births |
>=6 Births |
|
| Child Immunization | 50% | 37% |
| Skilled Antenatal Care | 66% | 50% |
| Pregnancy Complications | 19% | 29% |
| Skilled Birth Attendance | 43% | 25% |
Source: PDHS 2007
One can also argue that factors including education and material resources affect fertility or have a bidirectional relationship. Education leads to lower fertility rates as indicated by Total Wanted Fertility and Unwanted Fertility Rates for the uneducated at 3.7 and 1.1 as compared to 1.8 and 0.5 for the higher educated. Additionally children especially girls with fewer siblings are more likely to enter and stay in school as indicated by the enrollment rate of 77% for girls with 2 or less siblings compared to 58% with 5+ siblings. For boys the difference is much lower. Thus fertility even impacts MDG 2 and MDG 3: eliminating gender disparity in primary and secondary education.

Dr. Zeba Sathar presenting
Exploring ways to lower fertility, Sathar put greatest stress on the need to delay or curtail unwanted fertility to improve maternal & child health. She argued that babies born with less than an 18 month BCI were much more likely to be undernourished and thus more prone to mortality. Additionally shorter intervals in successive births lead to higher mistimed and unwanted births. For an interval of < 1 year, mistimed and unwanted births are 23% and 16% respectively, for 2 years they decrease to 17% and 17% while for a period of 3 years they further decrease to 9% and 16% respectively.
Maternal and child health implications of shorter intervals were further explored by Dr. Ghazala Mahmud, who argued that the main cause of maternal mortality was too many births, too short an intervals and the mother’s age group- too young or too old. She suggested an “Optimal Birth Spacing Interval” (OBSI – time period between births associated with the healthiest outcomes for pregnancies, newborns and mothers) stating that World Health Organization (WHO) had suggested a birth spacing interval (interval from one birth to the next) of 2-3 years while US Aid recommends 3-5 years. Instead, in Pakistan 75.5% women gave birth in less than 36 months after the last birth. Though her chart reflected that mother morbidity (Third Trimester Bleeding, Anemia, Premature rupture of membranes, Puerperal Endometritis) and mortality drastically decreased by an 18 month birth to birth interval, perinatal outcomes presented a different picture as birth to pregnancy interval of < 18 months and > 59 months increased the risk of pre-term births and low birth weights. Data suggested that relative risk of dying (Adjusted Odds Ratio) decreased from 3.87 to 1 when the interval increased from < 24 months to a period of 36-47 months.
She further quoted from research literature how pregnancy within 6 months of a live birth leads to 650% higher risk of induced abortion, 150% of maternal death, 70% of pre-term birth, 230% of miscarriage and 220% higher risk of infant mortality. Similarly pregnancy soon after miscarriage or abortion carries an increased risk.
Katie McDonald while agreeing with Sathar on the need to curtail fertility furthered Mahmud’s point by arguing for Healthy Timing and Spacing of Pregnancy (HTSP) strategy which goes beyond OBSI’s fertility reduction focus, instead concentrating on the role of contraception for healthy pregnancy outcomes and healthy fertility. Quoting results of HTSP programs in Egypt (2003-2005), where CPR increased from around 50% to 80%, she articulated that family planning increased substantially in a relatively short period of time when families learnt of pregnancy delay and spacing being associated with greater health for the mother and infant.
There was an overall consensus that limiting fertility by increasing birth intervals and fulfilling unwanted pregnancies was imperative to improve maternal and child health. In addition it improved outcomes for children education and gender equality. The suggested strategy of HTSP primarily reorients FP from a numbers game to a health intervention making it a need for a healthy mother and child. This could also be the only way to convince the recipient, the man and the family to decrease fertility. But it is not enough to counter societal pressures to have a child within three months of marriage or to require a boy child.
The suggested HTSP strategy should include advocacy,
“Limiting fertility by increasing birth intervals and fulfilling unwanted pregnancies was imperative to improve maternal and child health.”
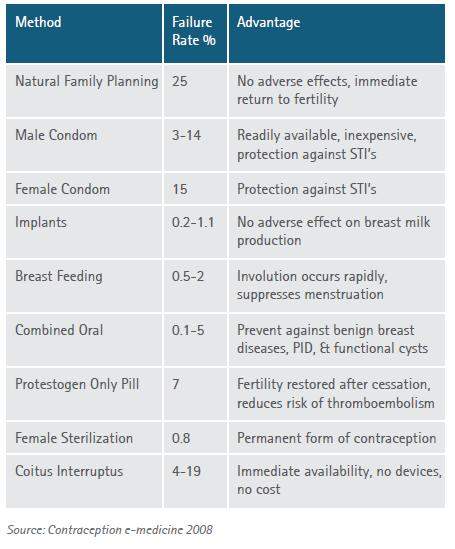
training and counseling linking child spacing and fertility to maternal and child health. Awareness of these issues needs to be raised among policy makers, families, men, the recipient and the marriageable age group. The current Behaviour Change Communication (BCC) programs lack publicity of risks & benefits of pregnancy spacing, availability of HTSP training material and awareness of optimal family planning methods. Only by raising the service delivery’s institutional capacity for antenatal counseling, postnatal clinic visits, evaluation & monitoring of birth spacing methods and knowledge collection around pregnancy & postnatal time period can family planning programs be transformed into the health intervention strategy required for better acceptability by communities.
: Optimal Contraceptive Methods
Citations